New York City is at the epicenter of the Covid-19 health crisis, and as a New York City-based College that educates students committed to public service, our alumni, students, faculty, and staff are working on the front lines to keep our communities safe. Our “Front-Line Heroes” article series serves as a testament to the valiant efforts of our first responders and essential workers. As a community we thank them for their service, dedication, and personal sacrifice.
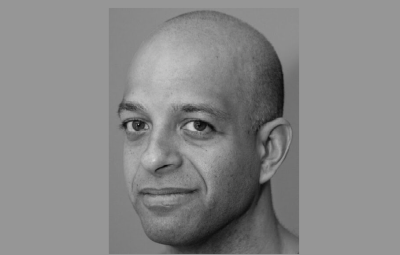
John Jay graduate student and first responder Khalid Islam ’20 is helping keep New Yorkers and the City’s first responders safe as they face the Covid-19 health crisis. As Emergency Medical Services (EMS) Safety and Training Manager for the Mount Sinai Health System his role has evolved from training and educating paramedics and emergency medical technicians (EMTs) so they can keep up to date with the state’s latest certification requirements, to more of a safety officer role ensuring first responders are properly protected on the front lines. “What’s making this Covid-19 pandemic a bit hard is that the guidelines and protocols are changing almost daily, sometimes multiple times a day,” explains Islam. “It’s part of my job to disseminate and explain that information to our providers and make sure that these are protocols that we can adhere to.” He’s also working as a paramedic part time, helping on the front lines in Brooklyn, New York. We spoke to Islam to learn more about the vital role EMS is playing on the front lines and how his John Jay training helped prepare him for this crisis.
“One of the key things that has to be done during a viral outbreak, especially one that’s new, is begin tracking. Tracking is fundamental to public health and emergency management.” —Khalid Islam
When did you start to see and really understand the impact that this virus was going to have on everyone’s lives?
One of the key things that has to be done during a viral outbreak, especially one that’s new, is begin tracking. Tracking is fundamental to public health and emergency management. So, when we started to hear the news about Covid-19, we began having conversations about tracking, protecting providers, and mitigating community spread. We began to note suspected Covid-19 patients within our coverage area, identifying travelers and people with suspected symptoms, and put these metrics on our patient’s electronic charts. These were marked by red flags. Our providers were also documenting people with symptoms, and these “flags” were automatically sent to us, our administrators, and physicians. As these metrics went up, we increased active protection and active protocols. Once we started to notice a large, exponential increase is when I realized this pandemic is here and it was going to spread. And in March, we could actually see from the data point that this was reaching a community spread.
What were your concerns when you realized the virus had started to spread?
For us, the biggest concern was trying to figure out the best way possible to protect our providers. How do I know where to direct our resources and forces when a virus can’t be seen? Pandemics are unique because you can’t physically see it. And because it’s invisible, unfortunately, a good portion of the public isn’t going to take it seriously. They aren’t going to react to something unless they can physically see it in front of them, or it’s affecting them on a personal level. And that’s what makes this extremely challenging.
“One of the biggest things we’re seeing is the affect this pandemic is having on our providers’ mental health. Our first responders are drained and overworked. They’re worried about their loved ones and worried about their home life.” —Khalid Islam
What does a typical day look like for you?
My full-time role is more logistics and safety observations, ensuring our providers have the resources they need and that they’re using the Personal Protective Equipment (PPE) correctly—I’m also active clinically as a paramedic part time. My typical day is spent reviewing charts to make sure our providers are protected, that they’re documenting what protective gear they were wearing during the patient call, and that they’re adhering to the changing guidelines. I’m also tracking our sick employees and providers, getting an idea of what they’re dealing with and pointing them toward resources that can assist them. One of the biggest things we’re seeing is the affect this pandemic is having on our providers’ mental health. Our first responders are drained and overworked. They’re worried about their loved ones and worried about their home life.
You mentioned you work part time as a paramedic. What has it been like for you working on the front lines?
It’s definitely tough being out there on the front lines. You’re going through the motions, putting on your mask, disinfecting the ambulance, wearing your PPE, but what I realized out on the field is that I can’t even be relaxed in my own ambulance. You’re worried all the time. You’re worried about getting infected. You’re worried about keeping a patient’s family members calm because they’re extremely scared and unsure of what to do. You’re trying to help the patient, and you’re also coordinating with other resources such as police officers, keeping them informed about the situation. It can definitely be overwhelming.
“I’ve worked for 10 years in the field as a paramedic. I’ve worked with paramedics and EMTs that have over 30 years of experience, and all of us agree that we’ve never seen anything like this before.” —Khalid Islam
What do you want our community to know about first responders working on the front lines of this global health crisis?
I want the community to really understand that EMS are an essential service and that our paramedics and EMTs are human. For some reason, EMS as a field has always been relegated as the “backup guys”—our efforts are never seen as heroic or essential. It’s really important to understand and remember, EMTs and paramedics are providing this vital service and they’re actively working to help communities. I’ve worked for 10 years in the field as a paramedic. I’ve worked with paramedics and EMTs that have over 30 years of experience and all of us agree that we’ve never seen anything like this. This is a tough experience for all of us. We’re human. We have the same fears and concerns as any other person. That human element, and the need for an essential service like EMS, is so important to remember.
How has your education from John Jay helped guide you during this crisis?
Last semester I took a class on responding to large scale disasters with Professor Lucia Velotti, Ph.D. One of the case studies we read about was the SARS outbreak in Toronto. We had to break down, discuss, and analyze this case. The SARS outbreak was almost a mirror image of what’s going on now with Covid-19. There were issues with space, issues with equipment, and issues with ventilators. There was so many missed opportunities because people weren’t taking the issue seriously and there was a breakdown in communications. So, once Covid-19 came on our radar state side, the big thing for me was to make sure there was an open line of communication with everyone around me, with our administration, with our medical directors, and our providers. I credit a lot of my John Jay courses with helping me get through this Covid-19 crisis because I’ve been able to apply a lot of what I learned in class on the field. And that’s the great thing about John Jay—they understand their students. They understand that students who work in public service and have hands-on field experience need knowledge and concepts that can be applied in the real world.
How has this global health crisis impacted you on a personal level?
It’s increased stress levels and it can be depressing. The protocol now is to resuscitate cardiac arrest patients out in the field. In the past, we were able to work up the patient and take them to the hospital. Now, if after 20 minutes, there’s no pulse, we have to pronounce them. So, when you have a higher incidence of cardiac arrest in the field, and you have to pronounce them dead in the field, that really starts to impact you.
“The losses of life are hitting all of us hard. We’re losing a whole generation of people and we’re not getting a chance to say goodbye.” —Khalid Islam
Is there any moment that hit you particularly hard?
The losses of life are hitting all of us hard. We’re losing a whole generation of people and we’re not getting a chance to say goodbye. I recently lost my mentor Anthony “Tony” Thomas, a wonderful paramedic who was a staple in New York City EMS for 30 years. Tony was one of the nicest guys you’d ever meet. He mentored thousands, including myself. He was a lung cancer survivor, a 9/11 first responder, and he was working full time up until he was hospitalized. I remember the day that Tony passed. Earlier that day I was working out of his location in Brooklyn and there was a get-well-soon card that we all signed for him. A few hours later, I learned he passed away and that hit me hard. Here we were getting a get-well card ready for the guy, and now we’re going to be including it in his casket.
Have there been any acts of kindness or moments that have uplifted you?
The community has really stepped up to show their support. We’ve received food deliveries from local restaurants, giving our providers the meals that they need to keep doing the job. A free meal means our providers don’t have to go outside and scramble to find food elsewhere. It’s touching to see New York City come together as a community to support our first responders.